A Commonly Overlooked Component In Unresolved Back Pain
In 1895, German physicist Wilhelm Conrad Roentgen discovered x-rays and radiographs. Soon thereafter, radiographs of the spine began to appear in prominent healthcare research and literature.
Later in 1916, Harvard Orthopedic Surgeon Robert W. Lovett, MD, published the third edition of his book Lateral Curvature of the Spine and Round Shoulders (1). This text has many examples of spinal radiographs, showing a biomechanical relationship between leg length, pelvic leveling, spinal scoliosis, and back pain.
4 decades later 1946, in the largest study at that time, Lieutenant Colonel Weaver A. Rush and Captain Howard A. Steiner of the X-ray Department of the Regional Station Hospital of Fort Leonard Wood, Missouri, meticulously exposed upright lumbosacral x-rays on 1,000 soldiers (2). The title of this study is:
A Study of Lower Extremity Length Inequality
American Journal of
Roentgenology and Radium Therapy
Vol. 51, No. 5, November 1946, 616-623
In this study, the authors Rush and Steiner constructed a spinal fixation and stabilization device to ensure the accuracy of upright measurements of leg length and their effects on spinal alignment.
Of the 1,000 soldiers in this study there were “consecutive, non-selected cases who were sent to the roentgen department because of a low back complaint.” By using their meticulous methodology of measurement, these authors concluded “it is possible to accurately measure differences in lower extremity lengths as manifested by a difference in the heights of the femoral heads.” The greatest difference in leg length measured was 44 mm, or about 1.75 inches.
As a result the authors made the following observations:
23% of the soldiers had legs of equal length.
77% of the soldiers had unequal length of their legs.
| Equal Leg Lengths | 23% |
| Short Leg | 77% |
| 1 – 5 mm Short Leg | 39.5% |
| 6 – 10 mm Short Leg | 22.5% |
| 11 – 21 mm Short Leg | 13.3% |
| More than 22 mm Short Leg | 1.7% |
The incidence of limb shortness was nearly equal between the left and right, and the average shortening was slightly more than 7 mm.
Importantly, concerning spinal biomechanical function, these authors also noted that the short leg was associated with a tilt of the pelvis and a scoliosis.
The authors also noted:
The roentgenograms were made in the upright position with the use of the stabilization device. Whenever there is a pelvic tilt, “there exists coincidentally a scoliosis of the lumbar spine.”
“Because this scoliosis, in all instances, compensates for the tilt of the pelvis, it is referred to by us as compensatory scoliosis.”
“The existence of this compensatory scoliosis in the presence of a tilted pelvis due to shortening of one or the other lower extremity is believed by us to have clinical significance and, furthermore, it is our opinion that the existence of any such condition cannot be determined with any degree of accuracy on gross physical examination.”
“Furthermore, it becomes immediately apparent that the making of roentgenograms of the lumbosacral spine in the recumbent position, as is frequently done, completely prevents the discovery of such pathology as this.”
“It was a general consistent observation that the degree of scoliosis was proportionate to the degree of pelvic tilt. An individual who has a shortened leg will have to compensate completely if he intends to hold the upper portion of his body erect or in the midsagittal plane.”
“A consistent observation which has been made is that in those cases with a shortened leg there is a corresponding tilt of the pelvis and a compensatory scoliosis of the lumbar spine.”
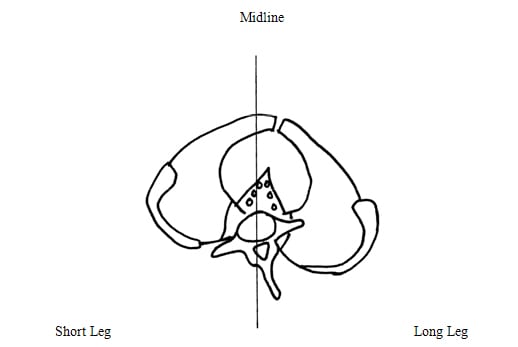
PLEASE SEE FIGURE #1
Of the 770 observed short leg cases seen in this study, only 8 had non-compensatory scoliosis.
These scoliosis deformities were associated with pathology such as bony changes from old trauma to the disc, facet, or vertebral body, and these authors defined them as structural scoliosis.
Leg length differences exceeding 5 mm were associated with greatest low back pain or disability, and therefore 5 mm is labeled as being a “marked difference.” The authors stated:
“For this reason, it is our opinion that the existence of such a condition [a short leg exceeding 5 mm] is significant from the standpoint of symptomatology and disability.”
Other findings noted in these 1,000 soldiers include:
| Sacroiliac Joint Arthritis | 5.5% |
|
Increased Lumbosacral Angle Above 50° |
4.3% |
| Lumbosacral Transitional Segment | 3.7% |
| Pars Defect With Spondylolisthesis | 2.7% |
| Reduced Lumbar Lordosis | 2.5% |
| L5-S1 Facet Tropism | 1.5% |
| Pars Defect But No Spondylolisthesis | 1.0% |
| L5-S1 Retrolisthesis | 0.6% |
An additional supportive article concerning differences in leg length, back pain, and scoliosis was published in the journal Clinical Biomechanics in November 1987, and titled (3):
The statics of postural pelvic tilt scoliosis; a radiographic study on 288 consecutive chronic LBP patients
Clinical Biomechanics
Volume 2, Issue 4, November 1987, Pages 211-219
The author, Ora Friberg, MD from Finland, exposed standing radiographs of the pelvis and lumbar spine in 288 consecutive patients with chronic low back pain and in 366 asymptomatic controls.
His important findings include:
| O – 4 mm Short Leg | 27% |
| 5 – 9 mm Short Leg | 30% |
| 10 – 14 mm Short Leg | 24% |
| 15 – 19 mm Short Leg | 10% |
| More Than 20 mm Short Leg | 9% |
“The incidence of leg length inequality in LBP patients (mean of 10.6 mm) was significantly higher than in 366 asymptomatic controls (mean of 5.1 mm).”
Consistent with FIGURE #1, in 91.4% of cases, “the lumbar curve was convex toward the short leg side, correlating significantly with the degree of lateral inclination of the sacrum and with the amount of leg length inequality. The curvature was generally coupled with an axial rotation of the vertebrae moving the spinous processes toward the concavity, as well as with an opposite rotation of the pelvis, which were calculated to result in a significant torsional stress on the L5-S1 segment.”
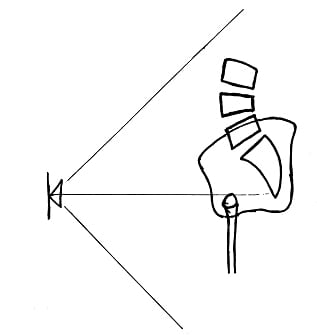
These “significant torsional stresses on the L5-S1 segment” are also well viewed in FIGURE #2 near the end of this months issue.
Other findings noted in the patients with chronic low back pain include:
| Spondylosis | 18% |
| L5-S1 Disc Degeneration | 12% |
| Spondylolisthesis | 8% |
| Spina Bifida | 7% |
| Lumbosacral Transitional Segment | 7% |
| Scheuermann’s Disease | 5% |
| L4-L5 Disc Degeneration | 4% |
| L5-S1 Retrolisthesis | 3% |
In both the studies by Rush/Steiner (1946) and Friberg (1987), a consistent observation is the association between an anatomical short leg and the presence of a compensatory scoliosis (See FIGURE #1).
Additional support for the short leg – scoliosis association was found by radiologist Augusto Manganiello, MD, and published in the journal Radiological Medicine in 1987 (4). The English abstract of this articles states:
“Following radiological investigations of the spine and pelvis, carried out in the standing position on 5000 young and adult subjects, the author reports a series of radiological features from which it appears clear that the inequality in length of lower extremities is the primary cause of that complex mechanism which is responsible of apparently idiopathic scoliosis.”
Thirteen years later, in 2000, Manganiello updates the understanding between leg length inequality and scoliosis by authoring a chapter in the book (5):
“Lower Limb Length Inequality And Scoliosis, in Etiology of Adolescent Idiopathic Scoliosis”
SPINE: State of the Art Reviews
Vol. 14, No. 2, May 2000
In this chapter, Dr. Manganiello notes:
“Among the causes of scoliosis, lower limb length inequality (LLLI) is certainly one of the most discussed and controversial.”
“During growth, LLLI, even of the order of just a few mm, can cause a tilt of the pelvis and consequently lateral deviation of the spine and head. The postural response, aimed at re-establishing equilibrium, is a compensatory counterdeviation of the spine.”
A compensatory counterdeviation that starts at L3 or above results in a gradual lumbosacral or thoracolumbosacral curve convex toward the shorter limb (FIGURE #1).
“In the treatment of scoliosis, the compensation of LLLI using a lift under the heel of the shorter limb is always useful and effective” in compensatory curves.
“The overload at the lumbosacral level may produce muscular stress, premature degenerative diseases of the disc or somatic structures and the interapophyseal joints L4-L5 and/or L5-S1, as well as dysfunction of the sacroiliac joint, which might give rise to low back and pelvic pain of mechanical origin.”
“Our findings suggest that LLLI can cause various curves, trunk imbalance, and asymmetric loading distributions. The overload at the lumbosacral level may produce structural changes of the spine and pelvis. These, modifying the orientation of the resting surface of the sacrum and the basal vertebrae, play a prominent role in the pathomechanism of scoliosis.”
In 1981, Giles and Taylor (6) add support between the association of leg length inequality and low back pain. Their article is titled:
Low-back pain associated with leg length inequality
Spine
Sep-Oct 1981;6(5):510-21
In this article, Giles and Taylor propose a meticulous in-office protocol for exposing upright radiographs to accurately measure the short leg and evaluate its effects of spinal biomechanics.
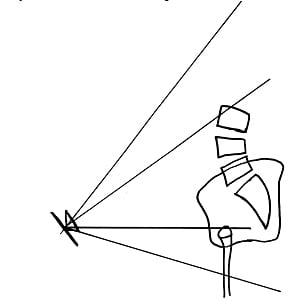
In their article, they stress that the most accurate measurement for the anatomical short leg requires an upright weight-bearing radiograph with the height of the tube placed as close as possible to the height of the femur heads (FIGURE #3).
A problem with this protocol is that much of the lumbar spine is not observable on the radiograph and therefore a lumbar spine biomechanical and compensatory scoliosis analysis is not possible.
Giles and Taylor therefore suggest tilting the x-ray tube cephalic (FIGURE #4), which will allow for lumbar spine and scoliosis biomechanical analysis without compromising the accuracy of the anatomical short leg measurement.
In 1983, physician Ora Friberg goes on to further detail the relationship between an anatomical short leg, back pain, and spinal biomechanics by exposing upright weight-bearing radiographs on 1,157 subjects. His article is titled (7):
Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality
Spine
September 1983;8(6):643-51
In this study, Dr. Friberg notes that leg length inequality became clinically relevant at 5 mm. Additionally, he states:
“Statistically highly significant correlations of the symptoms and leg length inequality were observed.”
In 79 % of those with chronic or recurrent sciatic pain, the symptoms occurred on the side of the longer lower extremity.
In 89% of those with unilateral hip pain, the symptoms occurred on the side of the longer leg.
“When correcting the leg length inequality simply with an adequate shoe lift, a permanent and mostly complete alleviation of symptoms was achieved in the majority of the cases,” which were followed up for at least six months.
In this article, Dr. Friberg details the importance of the counter-rotational stresses that the anatomical short leg imparts to the L5-S1 disc. Once again, this is best visualized in FIGURE #2.
Correction Of Anatomical Short Leg For The Treatment Of Back Pain
In 1970, physicians Bernard Sicuranza, Joseph Richards, and Lislie Tisdall published a study entitled (8):
The Short Leg Syndrome in Obstetrics and Gynecology
American Journal of Obstetrics and Gynecology
May 15, 1970, Vol. 107, No. 2, pp. 217-219
These authors are from the Department of Obstetrics and Gynecology, St. Mary’s Hospital, Brooklyn, New York. They note that an anatomical short leg can cause chronic low back and flank pain, and that “many women had been subject to hysterectomy, uterine suspension, and presacral neurectomy with poor results.”
The pain is because of imbalance causing traction on the abdominal, paravertebral and gluteal muscles. The pain is “increased when standing, during exercise, and after physical exertion, and is generally relieved by rest.”
These authors found that treatment consisted of the “application of a lift to the heel of the short leg.” “Relief was usually prompt and in most instances no more than 2 weeks is necessary for complete adjustment. The results of applying a heel lift on the short leg were excellent in 90% of the patients.”
In 1985, rheumatologist J. Philip Gofton, MD, published a study entitled (9):
Persistent Low Back Pain and Leg Length Disparity
Journal of Rheumatology
Vol. 12, No. 4, August 1985, pp. 747-750
Dr. Gofton notes short leg caused low back pain is a chronic problem that comes on within 20 or 30 minutes of being upright, and is relieved quickly with sitting. Dr. Gofton states that the best treatment is the insertion of an appropriate heel lift.
Additionally, he notes:
“The notion that low back pain may be caused by minor leg length disparity is plausible.”
“The suggestion that leg length disparity can produce low back pain has been known since before the turn of the century and although lip service has been paid to it by physicians it is not a matter taught in medical schools nor addressed seriously by most physicians.”
“A radiological method in which the femoral head heights are measured on an AP radiograph of the pelvis taken in the erect position has shown to be reproducible.”
“Medial cartilage degeneration on the long [leg] side has been observed. Pain at the greater trochanter is often observed with discrepancy. Patients have commented that a troublesome ache at the base of the neck was improved together with their chronic low back pain, presumably because there is a secondary compensatory scoliotic curve in that area. One patient in the series, a physician, had a recalcitrant plantar wart which defied all treatment until his disparity was corrected. His back pain and the wart disappeared. Both reappeared when he omitted the lift to his shoe a year or two later and both disappeared on resumption of the correction. The probable effect of leg length disparity and a form of osteoarthritis of the hip has been documented. These observations suggest that distorted biomechanics and stresses throughout the body produced by what would initially seem to be a trivial asymmetry deserve more searching investigation.”
Also in 1985, rheumatologist Michael Helliwell published a paper based
upon 20 patients with leg length inequality and chronic low back pain. The title of his article is (10):
Leg Length Inequality and Low Back Pain
The Practitioner
May 1985, Vol. 229, pp. 483-485
In this article the author notes:
“A permanent shoe raise to the shorter leg improved the symptoms in the majority of the patients.”
“This supports the view that leg length is a readily identifiable and easily correctable cause of chronic back pain.”
The most interesting article pertaining to leg length inequality and chronic back pain was published by Ruth Defrin and colleagues in 2005 (11). Their article is titled:
Conservative Correction of Leg-Length Discrepancies of 10 mm or Less for the Relief of Chronic Low Back Pain
Archives of Physical Medicine and Rehabilitation
November 2005, Volume 86, Issue 11, pp 2075-2080
These authors note:
“Several researchers have suggested that leg-length discrepancy (LLD)—that is, a disparity of length between the legs—might also be a cause of LBP.”
Leg-length discrepancy (a disparity of length between the legs) is a cause of chronic low back pain.
Mild leg-length discrepancy of 10 mm or less is common, found in 96% of the adult population.
Leg-length discrepancy as small as 2 mm can be clinically significant.
Shoe inserts significantly reduced both pain intensity and disability in patients with chronic low back pain and a short leg of 10 mm or less.
Leg-length discrepancy causes asymmetry in the lower-extremity joints and in the spine and pelvis, leading to stress and strain with a derangement of normal biomechanical function, postural scoliosis, stress on facet joints and discs, resulting in degenerative changes.
These researchers initially inserted a 2 mm shoe lift, and increased the height by 2 additional mm every other day until the desired height was obtained.
“Patients of the control group who did not receive shoe inserts did not have any changes in either LBP intensity or disability scores.”
In this study, 96% of those treated with a shoe insert for chronic low back pain achieved complete pain resolution or significant pain resolution within 12 weeks.
Clinical methods of measuring leg length with a tape measure have low accuracy, reliability, and validity, and therefore are not suitable.
Shoe inserts are recommended to be included in the treatment of patients with chronic low back pain when they have mild leg-length discrepancy.
The final study is this report was written by physical therapist Yvonne
Golightly and colleagues from the Veterans Medical Center at the University of North Carolina in 2007. The title of their article is (12):
Changes in Pain and Disability Secondary to Shoe Lift Intervention in Subjects With Limb Length Inequality and Chronic Low Back Pain
Journal of Orthopaedic & Sports Physical Therapy
Vol. 37, No. 7, July 2007, pp. 380-388
In this study, these authors make the following observations:
Limb length inequality (LLI) may be a cause of low back pain (LBP).
Patients with LLI often have increased pain from standing for 20 to 30 minutes, followed by immediate relief upon sitting.
Multiple studies report higher prevalence of LLI in individuals with LBP compared to control subjects.
Clinical (non radiographic) methods to detect LLI have less reliability and validity than radiographic methods.
Evidence to support the association between LLI and LBP is provided by studies showing significant improvement in patient’s low back symptoms following insertion of a shoe lift.
Clinical methods to measure LLI are associated with error. The mean error magnitude in this study was 4.7 mm, with an upper range of 13.5 mm.
“Radiographic methods are the gold standard for measuring LLI, as compared to clinical methods.” The best radiographic protocol for assessing LLI includes the following steps:
- A carpenters level is used to ensure the floor is level.
- Subjects stand with equal weight on each foot.
- Both knees are fully extended.
- The feet are positioned so that the distance between the ankle joints are nearly the same as the distance between the two anterior superior iliac spines.
- The central ray is positioned within 20 mm (less than 1 inch) of the upper level of the most superior femoral head. [Essentially, the central ray has to be as close as possible to the height of the higher femur head]
- The difference between the most superior aspect of the two femur heads is measured to the nearest millimeter.
Full-length shoe lifts are superior to heal lifts alone, as long as the shoe can accommodate the full-length lift.
Elevated shoe lift height should begin at 1/8 of an inch (3.18 mm). The height of the shoe lift should be increased in increments of 1/8 inch every 7 to 14 days until optimum height is obtained based upon patients symptomology.
Patients with structural scoliosis require additional time (more than 2 weeks) to accommodate to the increase in shoe lift height.
The total amount of LLI should not be corrected, and the patient should determine the lift height based on their response to gradual lift intervention. In this study, the average show lift used was 61% of the radiographic measured LLI.
Patients should not use a lift that exceeds the magnitude of their LLI.
Typically, the reduction in chronic LBP pain and improvement in function was noted approximately 1 week following establishment of final lift intervention height.
The lift therapy used in this study “had positive results for most subjects and was implemented at relatively little cost.”
Previous long-term (up to 15 years duration) shoe lift studies for patients with chronic LLI “reported significant long-term improvements relative to relief of low back symptoms.”
“Shoe lifts may reduce LBP and improve function for individuals who have chronic LBP and an LLI.”
References
1) Lovett RW, Lateral Curvature of the Spine and Round Shoulders, third edition, P. Blakiston’s Son & Co. Philadelphia, 1916.
2) Rush WA and Steiner HA, A Study of Lower Extremity Length Inequality, American Journal of Roentgenology and Rad. Therapy, Vol. 51, No. 5, November 1946, 616-623.
3) Friberg O, The statics of postural pelvic tilt scoliosis; a radiographic study on 288 consecutive chronic LBP patients; Clinical Biomechanics
Volume 2, Issue 4, November 1987, Pages 211-219.
4) Manganiello A. Rilievi radiologici nelle scoliosi idiopatiche; Radiol Med (Torino). 1987 Apr;73(4):271-6.
5) Manganiello A; “Lower Limb Length Inequality And Scoliosis, in Etiology of Adolescent Idiopathic Scoliosis” SPINE: State of the Art Reviews; Vol. 14, No. 2, May 2000.
6) Giles LG, Taylor JR. Low-back pain associated with leg length inequality; Spine. 1981 Sep-Oct;6(5):510-21.
7) Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality, Spine. 1983 Sep;8(6):643-51.
8) Sicuranza B, Richards J, Tisdall L; The Short Leg Syndrome in Obstetrics and Gynecology; American Journal of Obstetrics and Gynecology; May 15, 1970, Vol. 107, N0. 2, pp217-219.
9) Gofton JP; Persistent Low Back Pain and Leg Length Disparity; Journal of Rheumatology; Vol. 12, No. 4, August 1985, pp. 747-750.
10) Helliwell M; Leg Length Inequality and Low Back Pain; The Practitioner; May 1985, Vol. 229, pp. 483-485.
11) Defrin R, Benyamin SB, Dov Aldubi R, Pick CG; Conservative Correction of Leg-Length Discrepancies of 10 mm or Less for the Relief of Chronic Low Back Pain; Archives of Physical Medicine and Rehabilitation; November 2005, Volume 86, Issue 11, pp 2075-2080.
12) Golightly YM, Tate JJ, Burns CB, Gross MT; Changes in Pain and Disability Secondary to Shoe Lift Intervention in Subjects With Limb Length Inequality and Chronic Low Back Pain; Journal of Orthopaedic & Sports Physical Therapy
Vol. 37, No. 7, July 2007, pp. 380-388.
Figure 1: Posterior to Anterior View From Behind
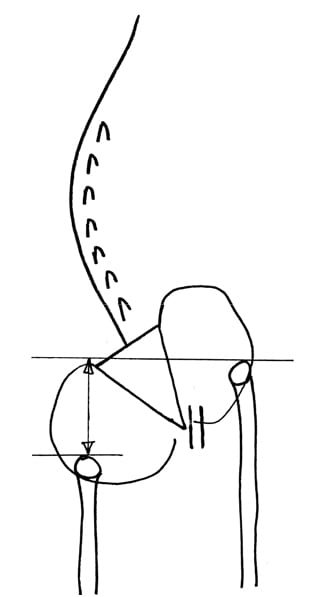
The left leg is short. The right leg is long.
The sacrum is lower on the side of the short leg (left in this drawing).
The spinal column initially tilts towards the short leg, then compensates back to the midline. Consequently, the spinal convexity is towards the short leg, and the spinal concavity is towards the side of the long leg.
The lumbar spinous processes (posterior) rotate towards the long leg. The pubic symphysis (anterior) also rotates towards the long leg. The consequent counter-rotational forces abnormally stress the L5 intervertebral disc.
Figure 2: Axial View From Above
The L5 spinous process has rotated to the right of midline, towards the side of the long leg. This causes a counterclockwise rotation of the L5 vertebrae and a counterclockwise rotation of the L5 intervertebral disc.
The pubic symphysis and pelvis has also rotated to the right of midline, also towards the side of the long leg. Because the pubic symphysis is in the anterior, this causes a clockwise rotation of the pelvis and sacrum, and a clockwise rotation of the L5 intervertebral disc.
These counter-rotational stresses primarily affect the L5 intervertebral disc. The consequences of these counter-rotational stresses at L5 are accelerated disc degeneration and degradation, back pain and sciatica.
Figure 3: Lateral View, No Tube Tilt
For best accuracy in the radiologic determination of the length of the legs, the height of the x-ray tube should be as close as possible to the height of the femur heads.
Figure 4: Lateral View with Tube Tilt
Tilting the x-ray tube does not alter the leg length analysis as long as the height of the x-ray tube remains as close as possible to the height of the femur heads. Tilting of the x-ray tube allows for biomechanical analysis of the entire lumbar spine.